IUDs and a little thing called consent
Issue #99: Doctors need to believe women's pain and respect their choices when it comes to their own bodies
Trigger warning: This is an important piece to read, but contains stories of abuse, suicidal ideation, abortion, and medical negligence. Parental guidance is advised for readers under 18.
Hello ji,
This week we are talking about a little piece of metal or plastic that can change a woman’s life.
But more importantly, we are talking about that other little thing called ‘consent’ - which is the difference that can make this change an amazing one, or a catastrophic one.
The small metal/plastic thingie is called an intrauterine device, or an IUD.
Some of you may already know about it. For the uninitiated, here are some highlights:
What you need to know about an IUD (Source: NHS.uk)
An IUD (intrauterine device) is a form of contraception.
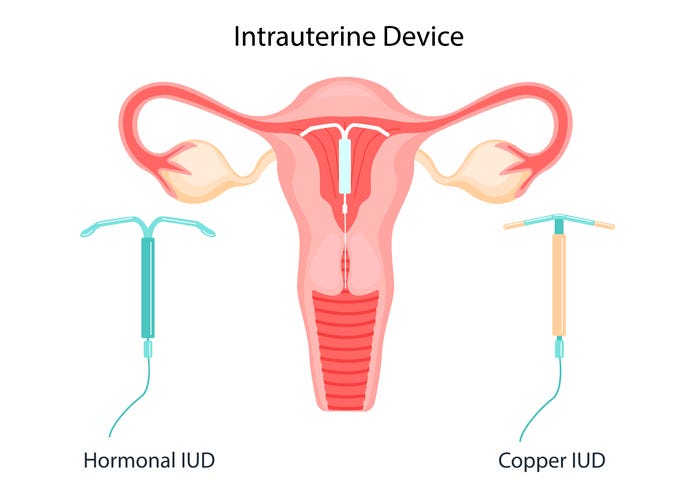
It is a small T-shaped device that is put into the woman’s uterus by a doctor. It comes in several types:
A Copper IUD, or a Copper-T, releases copper which protects against pregnancy for 5-10 years.
A hormonal IUD (e.g. the brand Mirena-T) is made of plastic and releases the hormone progestogen (synthetic progesterone) to avoid pregnancy for 3-7 years.
When inserted correctly, an IUD is more than 99% effective in preventing pregnancies.
An IUD does not protect against sexually transmitted infections (STIs), so it does not replace condoms in that sense.
An IUD works as soon as it is put in. It can be put in at any time during the woman’s menstrual cycle, as long as she is not already pregnant (this is crucial as we will see later in this piece).
It can be uncomfortable or painful when the IUD is put in, and women are advised to take painkillers later if they feel the need.
It can be taken out at any time, but only by a specially trained doctor. Once it is removed, it is possible to get pregnant straight away.
Possible side-effects:
After placing an IUD, the woman’s periods can be heavier, longer, or more painful in the first 3 to 6 months.
Spotting or bleeding between periods.
Small risk of an infection in the uterus, or a UTI.
Mood swings, skin problems, hair loss, and/or breast tenderness.
A decade of avoidable pain
Farah always had incredibly painful periods.
“Right from the time I hit puberty, the pain has been so debilitating that I would be at home, doubled up in pain, crying through every period.
It got worse through the years. Every doctor I saw told me that the solution was to have a child. The usual questions would go ‘Are you married?’ When I said ‘no’, they would say, ‘Why not? Get married, have a child, and everything will be okay.’
When I was single, they would say, ‘Get your mother - I will talk to her about this’. This happened to me even when I was a 24 years old woman!
After I got married, it became ‘Get your husband - I will talk to him about this’.
Basically, I had no choice and no agency in their eyes - not even when it came to my own body.”
But Farah did not want a child.
“Never did, still don’t. I love my life the way it is. I married at the time I wanted, and to the person I wanted. I refused to make the life-altering choice of having a child I did not even want - just as a Hail Mary that might or might not cure my gynaec problem. I tried many doctors and they all wanted to talk about my marriage instead.
You’d think I was going to them for marital advice, and not medical advice!”
In the meantime, Farah’s pain became intolerable. By the time she was in her 20s, she could literally not move when on her period.
“But every doctor I saw about it clearly thought that I was a delicate woman, making a big deal of a minor discomfort. In truth, I have an extremely high threshold for pain. But how do you convince someone of something as inexplicable as pain - especially when they have already decided not to believe you?
After seeing several such disappointing doctors, I gave up and accepted that it would be my fate to have to live my entire life like this.”

Can you imagine living like that? To not be able to function five days a month, every month, your whole life? Farah paints a vivid picture of what that looks like.
“Imagine having to call someone at your workplace - sobbing uncontrollably - to tell them that you are in so much pain because of your periods that you cannot come to work for the next five days.
Embarrassing, right?
I had to make that call every month.
I could never hold down a permanent job. I had to keep working as a freelancer because no job would offer the amount of leave I needed to take. My periods were running my career.
They were also running my personal life. I could never even plan a trip, or even a lunch with a friend because ‘what if I get my period around that time, and I can’t make it?’
It was an impossible way to live.”
Along with the pain came an insane amount of blood loss. When she was 30, Farah lost so much blood on her period one month that she had to be rushed to the hospital for blood transfusions.
“The doctor took one look at the sheer amount I was bleeding and immediately ordered tests for cancer. I was petrified. But then, the tests came back negative.
That was the first time a doctor believed - in the face of irrefutable facts - that I just had such horrible periods that it literally seemed like I had cancer.
That was also the first time that they actually investigated my condition. Some simple tests revealed cysts in my uterus. I was relieved at finally having an explanation.
I told them to simply take the uterus out because I just could not live like this anymore.”
The doctors refused to do it, saying Farah was too young.
“I felt like all hope was lost. But then, a doctor asked if I had considered getting an IUD.
I had never even heard of an IUD. The doctor said that while the IUD is a contraceptive device, it might help my problem. Also, most women stop getting periods altogether with an IUD is inside them.
I could imagine no better reality than a life without periods.
I went for it immediately. And my life changed.”
In the following months, Farah experienced - for the first time in her life - the kind of freedom that most other women (and all men) feel.
“I was no longer writhing in pain five days a month. I am 45 years old today. I still don’t have a child, and I am very happy with my decision. It has been 15 years, and I get my IUD replaced regularly. I cannot imagine life without it.”
Farah loves her IUD. But wonders if it was necessary for her to suffer such debilitating pain for over a decade to get to it.
“The IUD saved my life. There is no doubt about it.
But looking back, I am filled with rage at the thought that I was forced to go through an entire decade of horrifying, debilitating, traumatic pain because none of my doctors treated me with the basic respect and trust a human being deserves. It took an actual cancer scare for them to even see my problem as a real one.”
“If a doctor had suggested an IUD when I was 20 years old, it would have saved me a decade of trauma. But all the gynecologists I saw were more focused on forcing me to have babies than on doing their jobs.”
“I wanted to end my life just to stop the pain”
Angel had a challenging childhood, made much much more difficult by her periods.
“I got my periods at 15. Soon afterward, my parents separated. It was not amicable and things got ugly. As the youngest child, I was pulled into opposite directions by my parents. I don’t know if that emotional stress contributed to how bad my period got, but I started bleeding 15 days a month. This went on for 6-7 months.
I dropped weight and started looking deathly pale. At one point, doctors suspected it was cancer. Then, they thought it was TB. Then, HIV. All tests were negative and no one could figure out why I would not stop bleeding.”
Eventually, someone recommended Dr. Rustom Soonawala in Mumbai.
“I fell in love with Rustom uncle instantly. He was the first doctor who actually treated me like a human being. He would actually address me directly, instead of talking to my parents as if I wasn’t in the room. He listened. Actually listened. That alone was such a relief, given that I was getting used to being treated as an inanimate object by my doctors by then.
He put me on birth control pills, saying that the hormones would help regulate my periods. The 15-days of bleeding stopped!”
While everyone was relieved that Angel had stopped bleeding and losing weight, her problems were still far from over.
“I hated the pills. They gave me nausea and bloating and horrible pain. Rustom uncle changed the pills, but it wasn’t working.”
Meanwhile, it didn’t help that things got infinitely worse on the home front.
“My parents’ relationship deteriorated further. I was my father’s favourite child. So my mother dragged me to another city against my wishes, just to get back at him. She would starve me and brutally abuse me physically, mentally, and emotionally. My brother would also beat me up. This went on for 1.5 years. One day, they hit me so hard that I got a hairline fracture in my skull. I ran away to escape them.
I was 17.5 years old - homeless, with no money, not even clothes. I found a job somewhere and rented a room. I earned barely enough to pay for rent so there was pretty much no money left for food.
When I was 20, I had to terminate a pregnancy with a shady doctor because I did not have enough money to go to a decent one.
Without proper nutrition and with all the stress, my health kept getting worse.
As the years passed, my symptoms got worse, and new symtpoms appeared. I started getting major mood swings. One moment I would be calm and the next I would fly into a murderous rage. I was lost and confused about what was happening to me.”

After a few years, Angel got married. She also started saving money to go back to see Dr. Rustom Soonawala about her continued gynecological problems.
“The day I went back to his clinic, I was given an appointment with his son, Dr Feroze Soonawala. I have to say, I have never met a better doctor or human being. I was in tremendous pain and crying when I met him. He was patient and kind.”
“One late night, I called him crying - I wanted to end my life just to stop the pain. He stayed on that call with me for two hours, counseling me. I had never experienced such kindness from a doctor before. He literally saved my life that day.”
Eventually, Angel decided that she would rather have her uterus removed than live with the pain.
“I had to plan my entire life and work around the pain, the bleeding, the mood swings, the headaches, and the backaches. I had no idea what having a normal life felt like. I told Dr. Feroze to cut my uterus out of me. But he did not want to do a major surgery I might not need.
That was the day he suggested a Mirena-T. I had got zero sex education so had no idea what an IUD even was. He explained it in detail. I was willing to do anything at this point, so I readily agreed.”
The procedure took no more than 10 mins, and Angel says it changed her life.
“It was the best thing that ever happened to me. For the first time in my life, I felt free. Free to travel, free to work, free from the pain, free from the mood swings!
I only had light spotting for a few days afterward, and it some digestive issues. Also, I would get a slight headache once in a while. But all that was a small price to pay for the relief I felt. Mirena was the best thing ever for me.”
Angel shared why she thought it was important to tell me her story.
“If even one woman or girl out there realizes that there are options and we don’t need to stay trapped, my pain would not have been in vain. The world is cruel enough - why not spread a little hope?”
“A masterclass in medical negligence”
The IUD may have been a lifesaver for Angel and Farah, but every woman’s experience with IUDs is not necessarily as positive.
Sadly, their experience with women’s doctors seems to be just as negative.
Dr. Janaki is a surgeon herself. She was clear that she only wanted one child. During her first pregnancy, she was living in Europe.
“Once I stopped breastfeeding, I found that I had excessive bleeding during my periods. I asked my Ob-gyn to place a Mirena-T so that I could live free from periods. She did and it helped with the bleeding.
But soon afterward, I started experiencing some major side effects.
It affected my sense of emotional wellbeing. I had massive mood swings, and no longer felt like myself. My breasts were constantly tender. My hair started falling so fast that I was in real danger of losing all of it.”
By this time, Dr. Janaki had moved back to India and was working at a hospital in Delhi. She went to a local gynecologist and asked her to remove the IUD.
“To my utter shock, she refused to do it! I was baffled. I reiterated that I had made the choice of putting in the IUD, and it was now my choice to take it out. But she did not seem to care what I wanted, and kept pushing me to wait till the side effects subsided. But they were only getting worse.
This was just the beginning. Almost every doctor I saw would lecture me on how the side effects would subside, or try to deflect to other possible causes.
They said it could be PCOS. They said ti could be a thyroid issue. I had already done all the tests they prescribed. Every test came back normal and it was clear that the IUD that was the source of my problems.
What’s infinitely worse, every doctor I met was condescending to me. As a doctor myself, I could only imagine how much more condescending they were towards women who did not have the medical awareness or agency that I did.
I have to say, I failed in the face of bad doctors. With all my medical access, I could not find a single gynae colleague who treated me like a human being.”
“I just needed a doctor who listened. This was a simple medical decision I had made about my own body. I knew all the facts and happened to have a Masters in medicine!
But doctor after doctor would gaslight me instead of doing the simple 5mins procedure I needed. Because God forbid a woman gets to make a choice about her own body!”
Dr. Janaki says that the problem in women’s reproductive healthcare runs far deeper than just bedside manner.
“Lack of respect for women’s bodies is a systemic problem in the medical and scientific community. I have now read about the thousands of women who experience the same symptoms I did with Mirena. You would not believe the sheer lack of research that goes behind design and launch of women’s health products. If IUDs were somehow meant for men’s bodies, you can bet your last dollar it would never have come to this.”
Dr. Janaki shared this article with me, which says that the FDA had received “nearly 100,000 different injury reports” from women who had got a Mirena-T.
Here is a glimpse of the kind of side effects these women reported:
“Women who had the Mirena IUD implanted increasingly reported experiencing complications with the device. Often the device migrated from its original position, causing a lot of discomfort and some instances of extreme pain. Once the device migrated, it wreaked havoc on internal organs by perforating some of them.
Women with the IUD also faced a high risk of Pelvic Inflammatory Disease (PID), which affects the uterus and fallopian tubes. Cases of ectopic pregnancy have also been reported. The IUD also caused benign ovarian cysts in some women.”
After almost a year of failing to convince her doctors to respect her wishes, Dr. Janaki finally got rid of her IUD removed by lying.
“I went to a new doctor and simply lied that I wanted a second baby. She removed the IUD immediately, no questions asked, no tests ordered.
Apparently, I have no agency over my body but the sound of a woman having a baby is the secret password that unlocks all ob-gyn doors.”
How the removal went is another horror story.
“I did not tell her that I was a super-specialist surgeon. I wanted to know how she would treat any other patient. Her office did not have stirrups, so I had to put one leg on a window ledge for the procedure. Then she put her entire hand inside me without a word of warning and grabbed my cervix. When I screamed in pain, she thought it was hilarious and actually started laughing and singing a song!
After the procedure was done, I came out and sat down in front of her waiting for her advice. I had read about the Mirena crash, which is a collection of side-effects experiences by women who remove a Mirena-T due to the resulting hormonal imbalance in the body.
It can include symptoms like mood fluctuations, depression, anxiety, headaches and migraines, trouble with weight gain, hairloss, vomiting, fatigue, acne, breast discomfort, reduced libido and fertility problems - basically a lot of the stuff I was hoping to get rid of. I wondered what advice she will have for me on managing any such symptoms I got after the removal.
But she just told me to get moving. No advice on possible side-effects, or pain management, or possible infections. No painkillers, no antibiotics.
It was a horrifying experience and a masterclass in medical negligence.”
The Copper Silver Gold standard of care
Mona grew up in a conservative family in a small town.
“In 2001, I had my first child. After the birth, I was sure that I did not want another pregnancy. But my husband used to refuse to wear a condom, and I had other pre-existing conditions because of which doctors would not prescribe pills.
My mother suggested an IUD (copper-T). She took me to her gynae and got the IUD placed in me. Honestly, I had very little knowledge about these things at the time. I thought that if it worked for my mother, it should be fine for me too.”
But shortly after getting the IUD, Mona developed an infection.
“I started getting an itch in my privates, there was some discharge, and it started paining. I went back to the doctor and she told me that my IUD had gotten infected. Nobody explained anything to me. Doctors in my town were not the type who would go out of their way to explain to women what was happening to their bodies. She just went ahead and removed the IUD.”
Mona, once again, tried asking her husband to start using condoms.
“He refused point blank. He convinced me that he would pull out in time.
Of course, that never works, and I ended up conceiving another child almost immediately.
I wanted to go for an abortion. But my in-laws would not allow it. There was hardly a 1.5 year gap between my two children.”
After the second child, another doctor suggested an IUD again.
“She said, ‘Maybe the copper one does not suit you, so you should try the silver one.’ I had no idea that a Silver-T was even a thing. It could have been just a way to charge me more money, but I was desperate and went ahead with it.
After the placement, I started getting UTIs (urinary tract infections) again. The doctor kept giving me antibiotics which would work for 2-3 months but the UTIs kept coming back.
The IUD was clearly not suiting my body. But I was petrified of getting it removed because the last time I did that, I got pregnant immediately.”
Knowing that she would get no support from her husband in terms of contraception, Mona kept living with repeated infections for four more years.
“The UTIs started getting serious. At one point, I was bleeding so much that they tested me for cervical cancer. Finally, my doctor told me that the infection would spread to other organs if I didn’t get the IUD removed right away. So I had to get it out.
After I got the silver-T removed, the issues with my husband resurfaced. Our sex life was horrifying for me. I was afraid of getting pregnant again and he staunchly refused to wear a condom despite knowing everything I had been through with other contraceptives.”
“My husband would force me to have sex without a condom, and after a few months, I could not take it anymore.”
Mona went back to her doctor and insisted that she put in the IUD again.
“I knew it would cause infections at best, and cancer or uterus damage at worst. But I was left with no other choice if I wanted to avoid another pregnancy.
This time, the doctor said she will move me to a Gold-T (which costed even more money). I was in a state of panic so I told her to go ahead.
Now, before the IUD procedure, doctors are supposed to do an ultrasound to rule out pregnancy. I don’t know if my doctor didn’t do it or didn’t do it properly - but she went ahead and placed the IUD inside me.
As soon as I reached home, I started feeling something very similar to labour pains. I went to the washroom and found that I was bleeding profusely. There was blood everywhere, and a mass came out of me. When I looked at it, I could clearly see a head and limbs. I realized to my horror that I had been pregnant without my knowledge, and the IUD had terminated my pregnancy.”
Mona immediately called her doctor, who denied that she had missed a pregnancy while placing the IUD. Mona had to take a photo of the foetus and send it to her to prove that she wasn’t lying.
“I don’t know how I found the strength to get through that night all alone.
I knew I could not share this with my husband or in-laws because they would allege that I intentionally aborted their grandchild. I somehow cleaned up all the blood in the bathroom, and rushed back to the hospital. It was midnight by the time I got myself admitted again for treatment of the botched-up IUD insertion and the accidental abortion.”
“All through this journey, my family was unsupportive. My husband was unsupportive. And my doctors kept gaslighting me.
When I was getting painful UTIs, they said that UTIs are common and I was overreacting to the pain. One doctor even told me I was going through menopause. (I was 30 years old at the time, and even had a pregnancy after that!)
And on the day she aborted my pregnancy due to her medical negligence, my doctor never apologized or even admitted the full extent of what she had done to me.”
“IUD-related coercion happens because doctors have a God complex”
Dr. Smita has observed and conducted multiple IUD insertions during her medical training.
“During our rural rotations, I have seen many women being coerced into getting an IUD after delivery because the doctor thought it was for her own good. This is not how informed consent is supposed to work.
Even during the procedure, the woman's pain is completely ignored. IUD insertion is a painful procedure and is usually done without any anesthesia. I have heard horrible stuff said to patients in pain, like ‘Sex karne mein to bada mazaa aata hai, toh is mein itna kya dard ka naatak? (You have a lot of fun having sex, so why so much drama around this pain?’”
Dr. Smita finds it ironic that she knows many women Ob-Gyns who would not opt for an IUD themselves.
“I have talked to multiple female obs-gyne residents who say that they would never get IUDs because they would not like to have something artificial inside their bodies. It is an understandable mental barrier in itself, but it is hypocritical when they force other women to get something they would not choose for themselves.”
Dr. Smita is personally a big supporter of IUDs.
“Let me say that IUDs are one of the best long-term, low-effort, highly effective, and reversible options for contraception out there. They work for many, many women.
In fact, in many cases, they can be a source of empowerment. Women often don't have reproductive choices in Indian households. I have seen many women secretly ask their ob-gyn to put in an IUD after their delivery, and not tell the husband or in-laws. The husbands and in-laws force women to keep reproducing until a boy is born. They don’t care about the toll multiple pregnancies take on a woman’s body. Also, many clinical studies have shown that IUDs are largely safe and becoming a popular contraceptive method, especially among younger women.”

Then why - I asked Dr. Smita - do doctors coerce women into getting IUDs? Why not gently counsel them and then let them make the decision for themselves? Isn’t a doctor who forces a woman to get an IUD as bad as her in-laws who force her to not get one?
“A lot of IUD-related coercion happens because doctors have this God complex that they know the best. It usually comes out of well-intentioned beneficence. But they forget that the other person has their own set of values, fears, and goals. She has a right to make decisions about her own body, even if we might disagree with her decisions.”
Dr. Smita also shared a perspective from the other side.
“While insensitivity to patients’ choices can be a personal trait, most doctors are well-intentioned victims of the overburdened healthcare system. When you have to do 10-20 IUD insertions every day on top of all the other patient consultations and deliveries, it is hard to muster compassion and patience.”
“I don't think this is a valid excuse for any sort of inhumane behavior, but I also understand that burnout causes people to behave in ways they wouldn't want to.”
I want to emphasize that this is not an anti-IUD piece.
The IUD worked for some women mentioned in this piece and did not work for others.
But the one thing all of these women had in common was that if they had found a doctor who actually listened to and believed what they were saying about their bodies and their choices, they might have been saved decades of trauma.
Many of the women I interviewed shared very positive experiences with their IUDs:
Like this one:
“After two kids, I did not like most of the birth control options I had. Condoms can break, I am not able to be regular with birth control pills, and birth control injections are painful and needed every three months. My husband refused to get a vasectomy and my doctor refused to do a tubectomy for me. When she told me about the IUD, I immediately loved the idea of having hassle-free long-term contraception. Placing the IUD, I faced zero pain, or bleeding – just a little discomfort. I have had it for over 10 years now, and had it replaced twice. Overall, my IUD experience has been a good one.”
Or this one:
“When I became sexually active, I considered all my options for contraception. I liked the IUD the best because it is 99% effective – more than condoms and pills. I picked Mirena because I remember feeling slightly more comfortable about a hormone-based contraceptive, and I had read that some women experienced heavier menstrual bleeding with the Copper-T. The insertion was painful but quick. It took a few days for the pain to subside. I cannot emphasize how liberating it has been since to be free from the monthly period! I don’t have to deal with cramps, I don’t spend money on pads/tampons, and I am free of the bleeding. Women often feel uncomfortable about this side effect, but the period is not necessary for women’s health, so I love it!”
I know these are comforting experiences to read, especially after the horror stories above.
The IUD in all the stories is the same device. What sets the positive stories apart is something very basic, and yet very rare - a non-judgmental doctor who offers all options to a woman and respects her choice about the one she picks.
So, no - This is not a pro-IUD or an anti-IUD piece.
It is a piece about how every human being deserves choices, counseling, and basic respect from their medical health practitioners. And how women are often denied this, especially when it comes to their reproductive organs.
This is also not an anti-doctor piece.
I have a reverential amount of respect for the medical profession. I truly think that anyone who dedicates their life to saving lives is a God.
The problem starts when doctors start believing they are Gods too.
Because, yes, doctors are over-stressed. Yes, our medical healthcare systems are crumbling. Yes, we put a woefully inadequate amount of resources into healthcare. And yes, it is hard to have a pleasant bedside manner when you are treating a hundred patients every day.
But women get slapped for screaming in pain during childbirth by their nurses and doctors. And I have never heard of a man being slapped for screaming in pain after an accident, no matter how overburdened his doctor is.
Why?
Because - for better or for worse - doctors are not Gods. They are human beings. And they carry all the social, moral, and gendered biases and blindspots that the rest of us mortals do.
Probably the biggest and most destructive blindspot is this basic truth:
The only person who should have a say in a decision about a woman’s body is the woman herself.
My only agenda with this piece is that I want readers to use it to think deeply about their reproductive health choices.
I want you to use this piece to make a list of questions to ask your doctor about these choices, and for you to know the red flags to watch out for in the responses.
Most of all, I want this piece to give women (and their loved ones) the courage to ask for what they deserve - a doctor who listens.
Mahima
❤️ Love Womaning? Show it by becoming a paid subscriber or getting yourself some choice Womaning merch.
🔥 If you are an aspiring writer - or even someone who just wants to make their emails shine - check out my storytelling course, which includes writing workshops and one-on-one mentoring to help you write better, write consistently, and launch your own newsletter.





I have to voice a bit of disagreement with the comment above. I work in Medical devices and there are systemic issues in healthcare for women.
It is not a matter as simple as “Change your doctor” when there is a systemic issue. Yes, you might get lucky and find the right doctor but this is hardly a reasonable expectation to have for how healthcare is managed. You shouldn’t have to get “lucky” to find a doctor who just listens, takes your healthcare concerns seriously and respects your medical needs.
This should be the bare minimum a doctor is trained to do with patient care.
As a medical device professional, I can tell you the Mirena IUD case was hardly an exception where large numbers of corroborating accounts and complaints by women were simply ignored. There is a massive case surrounding transvaginal mesh implants that for years the company tried to just brush off. Little testing for done when it’s use was expanded from use for hernia and incontinence to female gynaecological conditions.
https://amp.theguardian.com/society/2017/aug/31/vaginal-pelvic-mesh-explainer
Lastly the choice to not use a condom or undergo vasectomy is a personal choice. Of course. But for too long the responsibility, pain and medical consequences of contraception have been easily relegated to women. When the female partner is unable to use available contraceptive methods, to still prioritize pleasure unconditionally over maternal health is selfish.
It is because culturally, all of this stuff has conveniently been placed in the “women stuff” bucket. Vasectomies are simple, highly effective. Yet uptake is limited in India because going through any inconvenience for family planning is considered needless by men.
It is time family planning and the associated medical processes for it be seen as a collective responsibility. Not some obscure feminine stuff.
aah the joys of seeing OB-GYN - I lived in India for 28yrs and I never saw a gynae or understood anything about female health or sexual health, beyond one sex ed class in school (which was so hush as if we were committing a crime). My mother never went to one until one because my father if our sickness was worth a doctors visit. When my sisters and I started menstruating, we were only taught how to wear a pad. And once I started dating, I became aware contraceptives.
When I moved to the UK and registered to the National Health System (NHS), the first thing they ask any female is about Cervical Cancer Screening - if you had one and how long ago was it (used to be called Pap Smear - https://www.nhs.uk/conditions/cervical-screening/). I had no idea what she was talking about, so she took the time to explain, gave me a pamphlet and asked me to make an appointment. They test you for it every 3yrs. It's the best preventive care.
Cut to several years later (still in the UK), I had severe pain in my in my lower abdomen and groin region every time I pee'd or poo'ed for over 3 months now, and much recently I had my periods twice that month. I called the GP and explained the problem. Simultaneously - I was talking to a private GP to get a referral for a gynae & understand what was going on. That process took 6 weeks because they thought it was Kidney Stones as I had a history for it, till they finally referred me to a gynae!
Doctor 1 ( male): When met him, he suggested a Transvaginal Ultrasound to check for cysts or growths. All was clearly explained, no issues here at all. The report said I had Endometriosis.
Endometriosis is a disease in which tissue similar to the lining of the uterus grows outside the uterus. It can cause severe pain in the pelvis and make it harder to get pregnant. Endometriosis can start at a person's first menstrual period and last until menopause. More on this, suggest to search and read on the NHS site.
My Endometriosis had been slowly growing for the past year and was 5cms big and every time I pee/ poo it touches my bladder and that's why it hurts. The doctor's advice was in the below order:
1. Do you want children? If so, now is a good time to get pregnant - explaining if your period stops, it will disappear.
2. Wait it out, it will get better.
3. Try over the counter pain killers.
4. Surgery, if you really can't bear the pain but this is not my usual practice place, so if you do choose surgery it will have to be 4 weeks from now.
Finally, as a by the by, you should consider losing some weight.
Doctor 2 (male) - my cousin, did another Transvaginal Ultrasound and said, I can't tell you what to opt for but given you are in pain and it's impacting everyday life, the easiest is a key hole surgery and you will recover within a week. (Then, he new to UK and was an NHS Doctor and didn't have a private practice so couldn't go through him for surgery).
Doctor 3 (Older female) - She said, could do surgery within 2 days but her recommendation was a Laparotomy Surgery (similar to a C-Section surgery - cut you open as if to remove a baby but remove the Endometriosis) instead of Laparoscopy (key hole) because the Endometriosis was now 7cms big. Grown in the last 2 months of figuring out which gynae to go and which doctor will give me sound advice and treatment.
By the time I saw the 3rd doctor, I was in so much pain, I opted for the riskier surgery - Laparotomy Surgery. Leaving me recovering with sick leave for 2 weeks & 4 weeks of work from home (this is pre-pandemic). Everything went well and I recovered well.
But some of the issues, I want to highlight:
1. Do you want children? If so, now is a good time to get pregnant - Pregnancy solves a temporary issue of a chronic disease like Endometriosis. So once I am done having the child, Endometriosis could come back. Also, one of the side effects of this disease is that you can't easily get pregnant. So if I wanted to have kids, I would struggle. But my spouse and I are clear we don’t want kids, so getting pregnant leaves us with a responsibility of a human being for the rest of my life, like WTF...
2. Wait it out, it will get better - This was the worst gaslighting. He assumed the pain is manageable without any medication or treatment and will go away on its own. I actually, did wait it out for a year & ignored my pain and the initial symptoms - low energy levels, constantly exhausted, and pain while having sex. I just thought it was me over working or some menstrual issue. Also, I have a high threshold of pain, I suffer from migraines frequently since I was 10yrs old, so going to a doctor generally is my last resort.
3. Try pain killers - Given frequent migraine issues, I was trying to avoid having daily pain killers especially since the doctor was vague on how painkillers would solve a superficial pain issue but not actually the core of the problem.
4. Surgery, if you really can't bear the pain but this is not my usual practice place so if you do choose for surgery it will have to be 4 weeks from now - Again stop telling me what I should feel, Yes, I can't bear the pain, its impacting my everyday life. And no, I am not waiting for you for a month for your schedule to be free.
5. Finally, lose weight - all of the above doctors mentioned, I try and lose weight - First, it’s very condescending because you don’t know what I have tried and what I am struggling with as you never asked me anything about my lifestyle. Second, I know lots of women who are thinner than me or even healthier and have had even worse case of Endometriosis than me. There is no scientific evidence that weight impacts Endometriosis - in fact 1 in 10 women in the UK suffer from this chronic issue and we don’t have enough clinical studies done to know the actual causes of this disease.